How VA is Advancing Prostate Cancer Care
Every year, approximately 15,000 Veterans are diagnosed and treated at VA for prostate cancer, and over 200,000 Veterans are prostate cancer survivors. VA is dedicated to addressing this cancer through evidence-based screening and providing the most advanced and effective prostate cancer care possible.
In support of its goal to advance prostate cancer care and treatment, VA has taken action, including:
Partnering with the Prostate Cancer Foundation to oversee prostate cancer centers of excellence at VA
Providing molecular testing for patients with metastatic prostate cancer
Increasing access to clinical trial participation
Developed a new prostate cancer clinical pathway
Prostate Cancer and the Cleland-Dole Act
In 2022, Congress signed into law the Joseph Maxwell Cleland and Robert Joseph Dole Memorial Veterans Benefits and Health Care Improvement Act of 2022, also known as the Cleland-Dole Act. In response to the Cleland-Dole Act, which requires VA to make strides in prostate cancer care, outcomes, and research, VA has published a prostate cancer clinical pathway and patient educational materials, and is in the process of creating a national prostate cancer registry.
Who should get screened?
For men ages 55-69 years, any decision to initiate or continue periodic prostate cancer screening with Prostate Specific Antigen (PSA) should be individualized. This is because screening offers a small benefit of reducing the chance of death from prostate cancer in some men. However, many men will experience harms of screening, including false-positive results that require additional testing and possible prostate biopsy; overdiagnosis and overtreatment; and treatment complications, such as incontinence and erectile dysfunction.
Routine screening for prostate cancer in men aged 70 and older is not recommended because the evidence shows that the harms of screening outweigh the benefits in this age group.
Some men should begin talking to their healthcare provider about prostate cancer in their mid-40s to figure out if they may be at increased risk for prostate cancer. Black male Veterans are encouraged to talk with their provider about their increased risk of developing and dying of prostate cancer, as well as the potential benefits and harms of screening.
You might be at increased risk if you:
- Have a family history of cancer especially those with a father or brother previously diagnosed
- Were exposed to Agent Orange or other environmental toxins
Before deciding whether to be screened, men should have an opportunity to discuss the benefits and harms of screening with their provider and to incorporate their values and preferences in the decision. Talk to your VA provider about whether prostate cancer screening is right for you.
Prostate Cancer Care and Treatment
Not all prostate cancer cases require treatment, but if you do, VA can support you through a diagnosis with access to the latest technology and approaches for individualized care. Treatment can be tailored to your unique genetic profile, helping you and generations to come. There are also options that can bring anti-cancer therapy to you.
VA uses a “hub-and-spoke” model for National TeleOncology, (NTO) with the main hub based in the Durham VA Medical Center. VA cancer specialists around the country work through NTO from their local VA Medical Center office, providing care virtually to a selected spoke site. Patients can connect with providers two different ways - they can either travel to a spoke site to connect with clinical video telehealth (CVT) or connect from their home using an internet-connected device with VA Video Connect (VVC).
- VA’s oncology experts have developed a prostate cancer clinical pathway, which uses current research to recommend the most effective, safe and cost-efficient treatments for Veterans with the least possible side effects, based on national guidelines and expertise.
- VA’s Precision Oncology Program for Cancer of the Prostate (POPCaP) provides Veterans with cutting-edge therapies for prostate cancer through a partnership with the Prostate Cancer Foundation and VA-sponsored clinical trials, such as the Prostate cancer Analysis for Therapy Choice (PATCH) program.
- The radiation oncology practiced across VA to treat prostate cancer is guided by best-in-class leaders in oncology, who are committed to providing high-quality care to Veterans. VA offers full-service oncology treatment that includes imaging, surgery, chemotherapy, radiation, and other advanced state of the art treatments as needed, either on site, or referred into the community. Additionally, VA patients are eligible for enrollment into clinical trials.
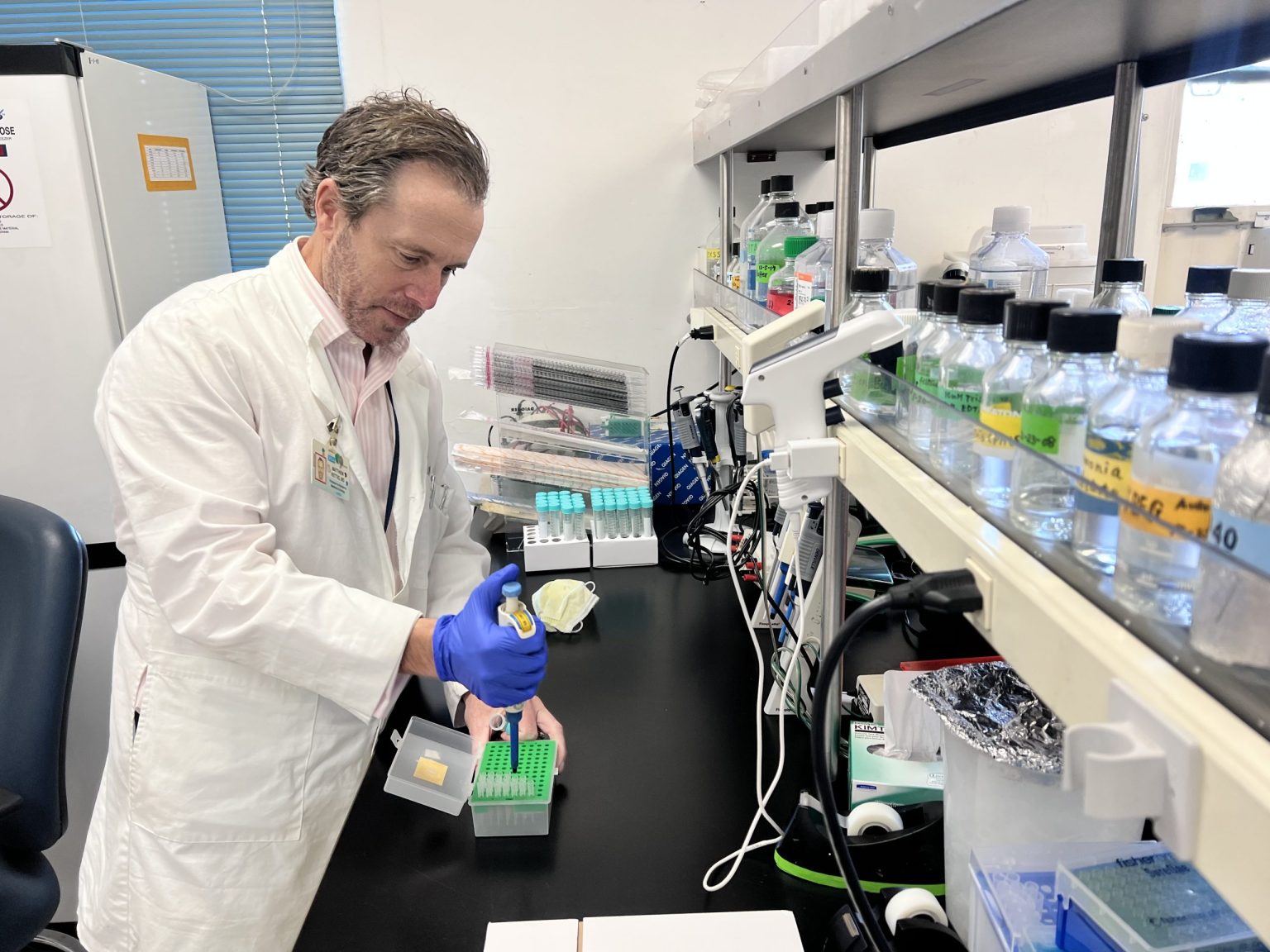
- Through the National Precision Oncology Program (NPOP), VA uses molecular testing to better select cancer treatment strategies for each individual Veteran, like Army Veteran John Hoose, featured in this video.
Wellness and Survivorship
Faced with the challenges of prostate cancer, maintaining well-being is of utmost importance. VA has transformative resources, guidance and real-world perspectives that empower Veterans, enhance well-being and foster resilience as they transition to cancer survivorship.
The Latest on Prostate Cancer at VA
New VA study to develop artificial intelligence that can predict aggressive prostate cancer
As part of a new research study that began July 1, five Department of Veterans Affairs medical centers are working together to develop an Artificial Intelligence algorithm that can predict if a case of prostate cancer might spread to other parts of the body.
Read More
Cancer care for American Indian and Alaska Native Veterans
At VA, our mission is to care for those “who shall have borne the battle” and for their families, caregivers and survivors. Our mission is your well-being. We’re committed to making sure all Veterans live their best lives and that includes prioritizing cancer screenings.
Read More
Better outcomes and better treatment: Equity in oncology for Black Veterans
What does equity in oncology mean? The positive impact of VA’s focus on health equity can be seen in the cancer care treatment outcomes of Black male Veterans. Prostate cancer is one of the most common diagnoses for the Veteran community.
Read More